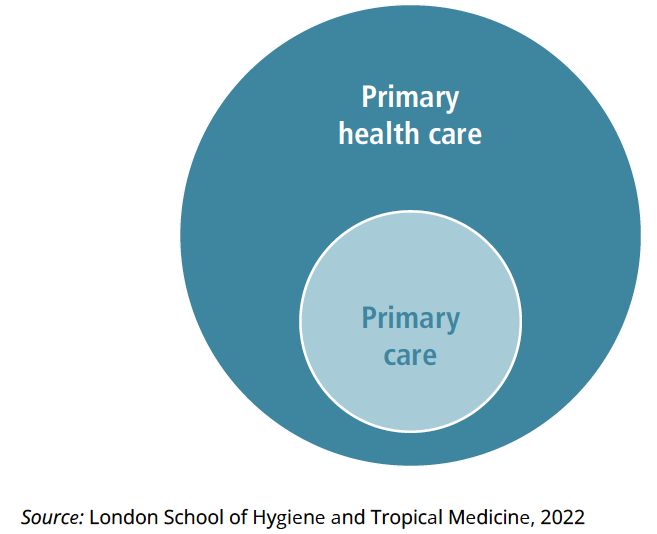
PRIMARY CARE AS A SUBSET OF PHC
A common approach to PHC implementation is to ground it in the development of strong primary care services that then build out to engage with communities and other sectors.
adpti.org
7/20/20243 min baca
Functional definition of primary care
The Declaration of Alma-Ata defines primary care as: “the first level of contact for the population with the health care system, bringing health care as close as possible to where people live and work. It should address the main problems in the community, providing preventive, curative, and rehabilitation services” (WHO, 1978). Building on this definition, Barbara Starfield articulated four characteristics of primary care, also well-known under the labels of four pillars, four tenets or simply the “4Cs of primary care” (Jimenez et al., 2021). They are “first contact, continuous, comprehensive, and coordinated care provided to populations undifferentiated by gender, disease, or organ system” (Starfield, 1994). Kringos et al. have further defined primary care as: “the first level of professional care service, where people present their health problems, and where the majority of the population’s curative and preventive health needs can be satisfied” (Kringos et al., 2010b).
First contact refers to primary care as “Comprehensiveness can be referred to as the “scope, breadth, and depth of primary care, including the competence to address health issues throughout the life course. Comprehensive primary care can respond to the majority of an individual’s health care needs, either through direct provision of care (for the vast majority of problems) or through referral to other levels of care or services” (WHO, 2018). Comprehensiveness in relation to the scope of services typically includes promotion, prevention, early diagnosis, curative, rehabilitative and palliative care (Jimenez et al., 2021). Comprehensive primary care has been associated with greater efficiency, improved care-seeking behaviours, better health and lower costs, predominantly via reduced unnecessary hospitalizations, increased uptake of preventive care, and reduced preventable complications (WHO, 2018; Jimenez et al., 2021).
Comprehensiveness can be referred to as the “scope, breadth, and depth of primary care, including the competence to address health issues throughout the life course. Comprehensive primary care can respond to the majority of an individual’s health care needs, either through direct provision of care (for the vast majority of problems) or through referral to other levels of care or services” (WHO, 2018). Comprehensiveness in relation to the scope of services typically includes promotion, prevention, early diagnosis, curative, rehabilitative and palliative care (Jimenez et al., 2021). Comprehensive primary care has been associated with greater efficiency, improved care-seeking behaviours, better health and lower costs, predominantly via reduced unnecessary hospitalizations, increased uptake of preventive care, and reduced preventable complications (WHO, 2018; Jimenez et al., 2021).
Continuity of care “results from the delivery of seamless coherent person-focused care over time across different care encounters and transitions of care” (WHO, 2018). It is distinct from, but related to, access and coordination, and involves an individual and a chronological dimension over time (Uijen et al., 2012). Three different types of continuity have been described: informational (the compilation of a person’s health information over time and across episodes in a single set of, or easily integrated, medical records, accessible as needed to various providers and increasingly, to users themselves); management (the consistent and coherent management of conditions over time); and relational (a sustained relationship between a patient or user and a clearly identified and accountable provider or team over the life course) (Haggerty et al., 2003; Salisbury et al., 2009; WHO Regional Office for Europe, 2010a). Relational continuity in primary care has been linked to better outcomes, improved cost– effectiveness, improved preventive care, fewer acute hospital visits and lower mortality, lower use of out-of-hours services, more personalized care and increased patient and provider satisfaction (van Walraven et al., 2010; Jimenez et al., 2021; Kiran et al., 2023).
Coordination refers to primary care’s responsibility to “coordinate service delivery across the whole spectrum of health and social care services, including mental health services, long-term and social care, through integrated, functional and mutually supportive arrangements (including referral systems) for transitions and information-sharing along evidence-based care pathways” (WHO, 2018). Through coordination, primary care helps patients navigate transitions between providers and settings of care, for example, providing support and follow-up after a person is discharged from the hospital. In PHC-oriented health systems, primary care is also responsible for the coordination of services between primary, secondary and tertiary care services; between physicians and other providers; between medical, preventive and social services; and between public and private services as required to address the specific health needs of a person (Jimenez et al., 2021).
Source: Implementing the primary health care approach: a primer(WHO,2024)
